Hydration in ADPKD: Can Water Slow Cyst Growth?
Medical Disclaimer
This article is for informational purposes only. It does not replace professional medical advice, diagnosis, or treatment. Patients with ADPKD should always consult a nephrologist or healthcare provider before changing their fluid intake. High fluid intake can be dangerous for certain conditions, including advanced kidney failure or heart conditions.
Hydration in ADPKD: A Simple Strategy to Support Your Kidneys
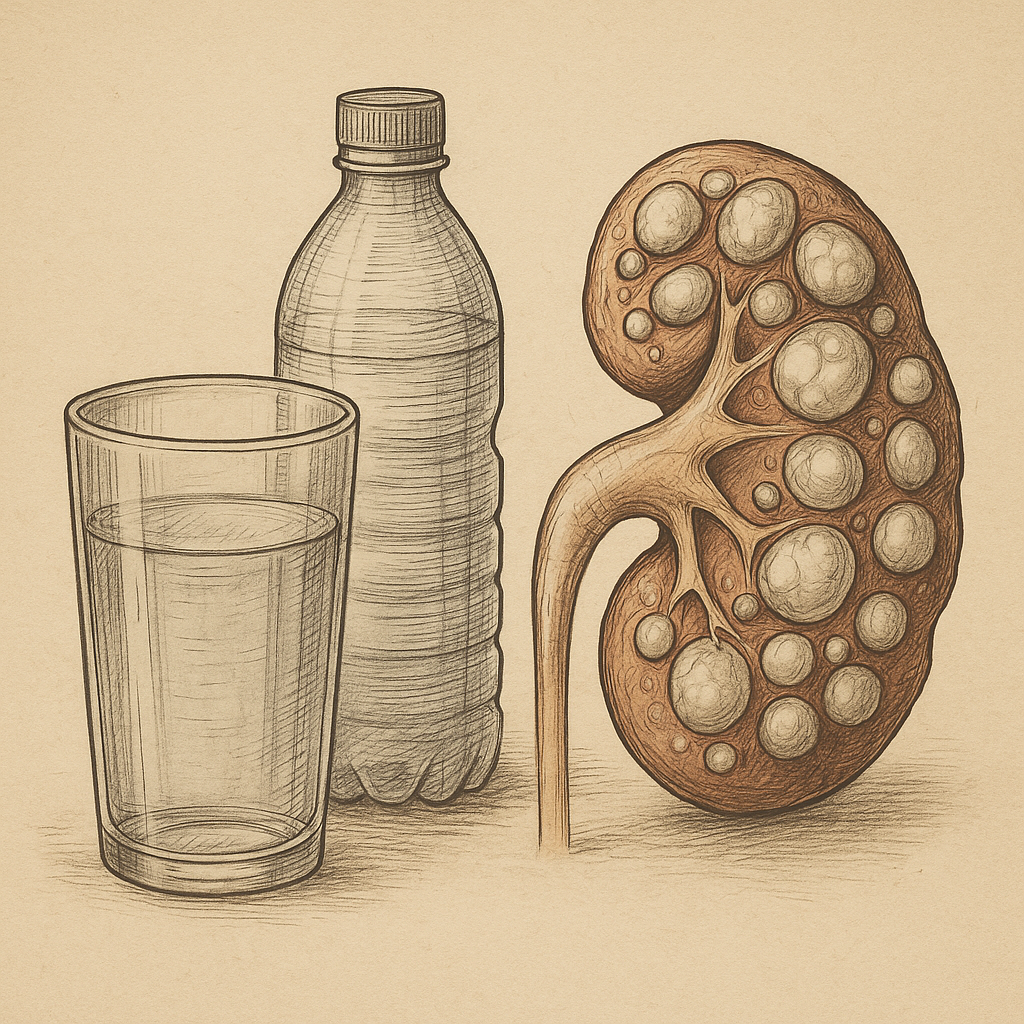
Autosomalna Dominująca Wielotorbielowatość Nerek (ADPKD) is the most common inherited kidney disorder, characterized by the progressive formation and enlargement of countless fluid-filled cysts in the kidneys. This relentless growth eventually leads to a decline in kidney function. While pharmacological treatments have emerged, patients are increasingly exploring accessible and non-drug strategies to manage the disease.
One such strategy is increased water intake, often termed “water therapy.” This simple lifestyle adjustment is built on a strong scientific rationale: by maintaining high hydration, patients may be able to suppress a hormone that actively encourages cyst growth. Understanding the evidence behind this approach—its feasibility, its effect on quality of life, and patient experiences—is crucial for making informed decisions about living with ADPKD [1, 2, 3].
Why Hydration Matters in ADPKD
The role of hydration in ADPKD goes far beyond basic thirst quenching. It directly intervenes in the hormonal signaling that drives cyst development.
The Role of Vasopressin in Cyst Development
In ADPKD, the growth of renal cysts is not a passive process; it is influenced by multiple factors, including a key hormone known as vasopressin (or Antidiuretic Hormone, ADH).
Vasopressin is responsible for regulating water balance in the body. When the body is dehydrated, vasopressin levels rise, signaling the kidneys to conserve water. Crucially, in ADPKD, this hormone also binds to receptors on the cyst-lining cells, stimulating two detrimental processes:
- Cell Proliferation: It encourages the multiplication of the cyst cells.
- Fluid Secretion: It promotes the secretion of fluid into the cyst, causing it to swell [1].
How Increased Water Intake May Lower Vasopressin Levels
The foundation of water therapy is to inhibit vasopressin release [1]. By consuming significantly more water, the blood becomes diluted. This dilution signals the body that it is adequately hydrated, thereby suppressing the production and release of vasopressin.
The clinical goal of this intervention is to maintain a state of low urine osmolality (meaning the urine is very dilute) throughout the day, effectively reducing the hormonal signal that stimulates cyst growth. This non-pharmacological approach offers a potential way to mitigate the progressive nature of the disease [1].
Evidence from Clinical Research
For a strategy as simple as drinking more water to be clinically accepted, it must be proven both effective and sustainable. Research has focused heavily on the practicalities and long-term acceptance of high hydration among ADPKD patients.
Feasibility and Adherence to Water Therapy Programs
Before large-scale trials on slowing disease progression can be run, researchers must confirm that the demanding fluid intake is feasible for patients in their daily lives. A clinical feasibility study showed that a protocol aiming for very dilute urine was indeed achievable for participants with ADPKD [1].
The study established that patients could safely maintain the prescribed increase in water intake when provided with the right educational tools and monitoring [1]. This finding is critical because it validates water therapy as a practical, viable, non-drug intervention that patients can realistically sustain [1]. The success hinges not just on the volume consumed, but on the ability to maintain the necessary low urine concentration over time [1].
Long-term Effects of Increased Water Intake on Quality of Life (HRQoL)
A major concern regarding water therapy is the impact of frequent urination (polyuria) on a patient’s Health-Related Quality of Life (HRQoL), potentially disrupting sleep, work, and social activities.
A long-term study specifically assessed HRQoL in patients maintaining increased water intake over several years [2]. The results were encouraging: sustained high water intake did not negatively affect the self-assessed quality of life measures [2]. Furthermore, the analysis revealed stable trends, and even suggested potential improvements, in specific domains such as the pain domain of HRQoL over the four years in the high-water intake group compared to the control group [2]. This suggests that patients can adopt this measure without severely compromising their overall well-being.
Patient Experiences and Perceptions of Maintaining Higher Hydration
Understanding the patient’s perspective is vital for long-term adherence. Another study focused entirely on participant perceptions, revealing the common challenges and motivations associated with this demanding lifestyle change [3].
Common Perceived Challenges:
- Polyuria (Frequent Urination): This was the primary disruptive side effect, especially during the night, leading to disturbed sleep [3].
- Difficulty with Volume: Struggling to consume and keep track of the large required daily volume of fluids [3].
Key Factors for Success (Motivation):
- Understanding the Rationale: Patients who understood that the water intake was directly suppressing the growth factor (vasopressin) were more motivated to adhere [3].
- Using Tools and Strategies: Patients successfully used reminders, planning, and specific timing strategies to manage the high volume [3].
These findings confirm that while commitment is required, the intervention is often perceived as worthwhile when the potential benefit of slowing cyst growth is clearly communicated [3].
Practical Guidance for Patients
If water therapy is recommended by a nephrologist, it must be approached with caution and individualized planning.
Personalized Hydration Targets
For ADPKD management, the target is not a fixed number of liters, but achieving a consistently dilute state of urine. This state is clinically measured by urine osmolality [1]. The required volume to reach this target is highly personalized and depends on:
- Body size and composition
- Dietary habits (especially salt and protein intake)
- Climate and physical activity level
- Remaining kidney function
Therefore, patients should never self-prescribe a high-volume regimen. The necessary volume must be determined and monitored by a clinician, typically through repeated urine testing, to ensure the therapeutic goal is met safely [1].
Potential Risks of Overhydration or Hyponatremia
While hydration is beneficial, excessive water intake, particularly in advanced stages of ADPKD where the kidneys struggle to excrete water efficiently, carries risks.
The most serious risk is hiponatremia (dangerously low blood sodium concentration), which can lead to symptoms such as nausea, headaches, confusion, or seizures. Patients must maintain a balanced electrolyte intake and closely follow the volumes specified by their healthcare team to avoid this serious complication.
Challenges and Limitations
While the evidence is promising, the research highlights areas that require careful consideration.
Differences in Adherence and Monitoring
Despite the general feasibility demonstrated, adherence to high fluid intake protocols can vary significantly among individuals [3]. Sustaining the rigorous monitoring required to ensure low urine osmolality over years is a considerable lifestyle challenge [1]. The current data suggests that educational and emotional support are key to overcoming these adherence hurdles [3].
Need for More Long-Term, Controlled Studies
Current evidence primarily stems from feasibility trials and quality-of-life assessments [1, 2]. While these are essential steps, the research still highlights the need for larger, definitive, and long-term controlled studies to confirm the direct impact of water therapy on the key clinical outcomes of ADPKD, such as Total Kidney Volume (TKV) and eGFR decline rate [1].
Takeaway: What the Evidence Suggests
Current evidence suggests that controlled, increased water intake is a safe, feasible, and sustainable supportive strategy for individuals with ADPKD [1, 2, 3].
Patients who understand the connection between high fluid intake and the suppression of the pro-growth hormone vasopressin are more motivated to sustain this lifestyle change [3]. The long-term quality of life data further reassures that this strategy can be integrated without unduly disrupting well-being [2]. Water therapy is a compelling example of how simple, accessible lifestyle modifications, when supported by strong scientific rationale, can complement complex medical management of chronic kidney disease.
FAQs About Hydration in ADPKD
Can drinking more water help slow PKD?
It may help by consistently lowering levels of vasopressin, a hormone linked to stimulating cyst growth. However, this therapeutic approach requires individualized monitoring and should be done under medical supervision [1].
How much water should I drink daily?
The amount is highly personalized and based on clinical goals, often guided by monitoring your urine concentration (osmolality), not a fixed volume. You must consult your nephrologist to set a safe and effective target [1].
Is high water intake safe for PKD patients?
It appears to be safe and well-tolerated in many patients, with stable long-term quality of life reported [2]. However, it carries risks (like hyponatremia) if unsupervised, especially with declining kidney function. Always follow clinical guidance.
What does vasopressin have to do with cyst growth?
Vasopressin binds to receptors on the cyst cells, encouraging them to multiply and secrete fluid, which causes the cysts to grow and enlarge the kidneys [1].
What makes water therapy challenging?
The primary challenge is adherence over time due to polyuria (frequent urination) and the necessity of monitoring and managing high daily fluid volumes [3].
References
- Feasibility of Water Therapy for Slowing Autosomal Dominant Polycystic Kidney Disease Progression. https://pubmed.ncbi.nlm.nih.gov/38556640/
- Long-term effect of increasing water intake on repeated self-assessed health-related quality of life (HRQoL) in autosomal dominant polycystic kidney disease. https://pubmed.ncbi.nlm.nih.nlm.nih.gov/39165901/
- Participant Perceptions of Increasing Water Intake in Polycystic Kidney Disease. https://pubmed.ncbi.nlm.nih.gov/40677362/
Related Reading
- What is Polycystic Kidney Disease? https://danielpindral.com/what-is-polycystic-kidney-disease/
No responses yet